Structure and Call Schedule
Lunch
- As of July 3rd 2023, residents on CUH MICU will pick up their food at the normal IM noon conference.
-
CUH Meal Card titled "Resident" will be funded for overnight shifts. CUH Meal Card titled "Internal Medicine Resident" will no longer be funded.
Team
- There are 4 teams with a total of 5 residents and 5 interns.
- Each team will consist of 1 resident and 1 intern.
- 1 resident and intern will be the night team assisting the on-call resident for 5-6 nights during the month.
- All residents and interns will rotate through night medicine during their month on service.
- Overnight team consists of the on-call resident, night resident and night intern. In addition, there is a night intensivist on call who should staff all admissions that come in overnight.
Hours
The day intern on call will admit patients until 5PM and check out to the night medicine resident between 6:30-7:00PM. The day intern on call must leave the hospital by 9PM. The day intern will then return the following morning by 7AM (no earlier than 5AM) and is expected to stay until all work is finished on post-call patients.
- Non-call Residents: 6:00AM-7:00PM
- Non-call Interns: 5:30AM-6:30PM
- On-Call Resident: 7:00AM-10:30AM (in the car by 11:00AM post-call)
- On-Call Intern: 5:30AM-7:00PM (Expected to receive check out and perform cross cover as first call for other teams until the night shift resident arrives)
- Night Shift Resident: 6:30PM-7:00 AM (unless primarily managing a critical event overnight - left up to the discretion of the resident - in which case you are asked to stay until the beginning of AM rounds to present directly to the attending)
- Night Shift Intern: 7:00PM-9:00AM (must be in the car by no later than 9:00 AM)
- On the night-float resident's / intern's last night, s/he should leave by 6 AM to ensure they have 24 hours off before returning to days.
Days Off:
- Resident: Post-post call
- Intern: Pre-call
Admissions
General admission guidelines
- Residents will admit from 7am - 5am the following day.
- Residents can NOT block admissions from the ED. The ER makes the decision regarding admissions to the ICU. Under rare circumstances, you may discuss the patient with your fellow or attending to discuss re-triage to another service. However, you are also responsible for discussing and coordinating transfer of care to the other service. You will remain responsible for the patient's care (labs, vitals, procedures, etc) while this happens. In this instance, you should leave a brief note in the patient's chart discussing your rationale for re-triage.
- If you are called about a floor patient who you do not think needs ICU care, you must involve the ICU fellow or the attending. If the attending or fellow believe the patient will be better served elsewhere, the MICU team is responsible for speaking with the other service to communicate the decision. You must speak with the attending or fellow before making this decision.
- Until the transfer and handoff to another service, you are responsible for the patient's medical care
- If an admission is called into the MICU on call resident between 5am and 7am, the off-going call resident is responsible for seeing the patient, stabilizing them, and putting in admission orders until they can hand off to the incoming call resident and intern. This is to prevent delays in care for these tenuous patients.
- Lack of beds should never play into your decision regarding a patient's admission to the ICU. If you are ever approached with a bed problem, notify your faculty member immediately.
- Insulin drips can be run on the floor.
- BMT patients require different approach to goals of care discussions than most patients. In general, avoid end-of-life discussions with these patients unless you have discussed your plans with the BMT team.
- Outside transfers/Zale Transfers/Service Transfers – These are also faculty decisions. Refer any calls or requests to your faculty (example: surgical resident calls you to transfer a patient to our service). Exceptions would be if the request comes from our consult fellows (moving from one ICU to another ICU service is not encouraged)
- Write a transfer note with current assessment and remaining goals and plans to assist the acceptance with care continuity
- Hospitalists accept patients up to 12noon daily. Do not call until patient is physically in a non-ICU bed.
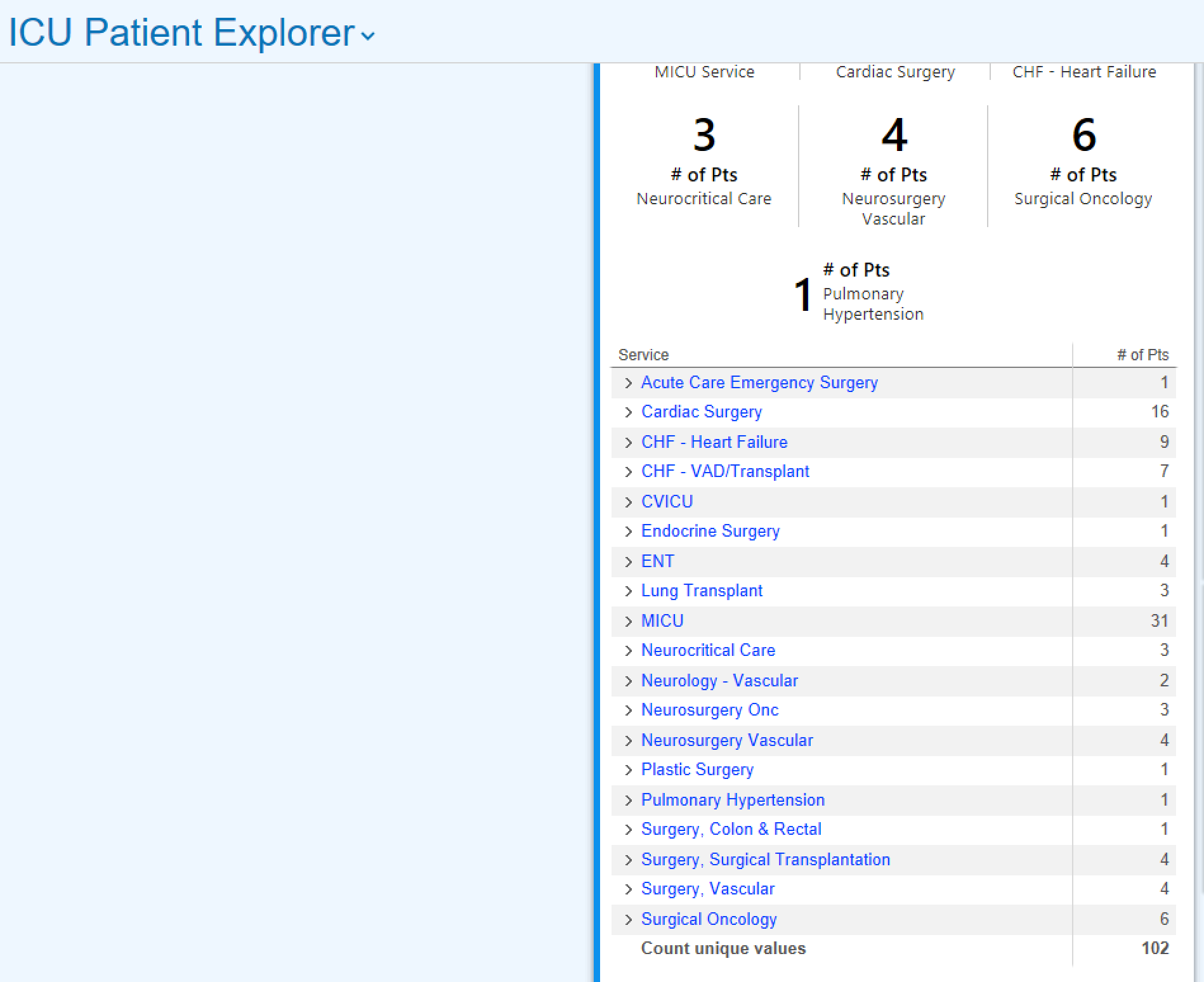
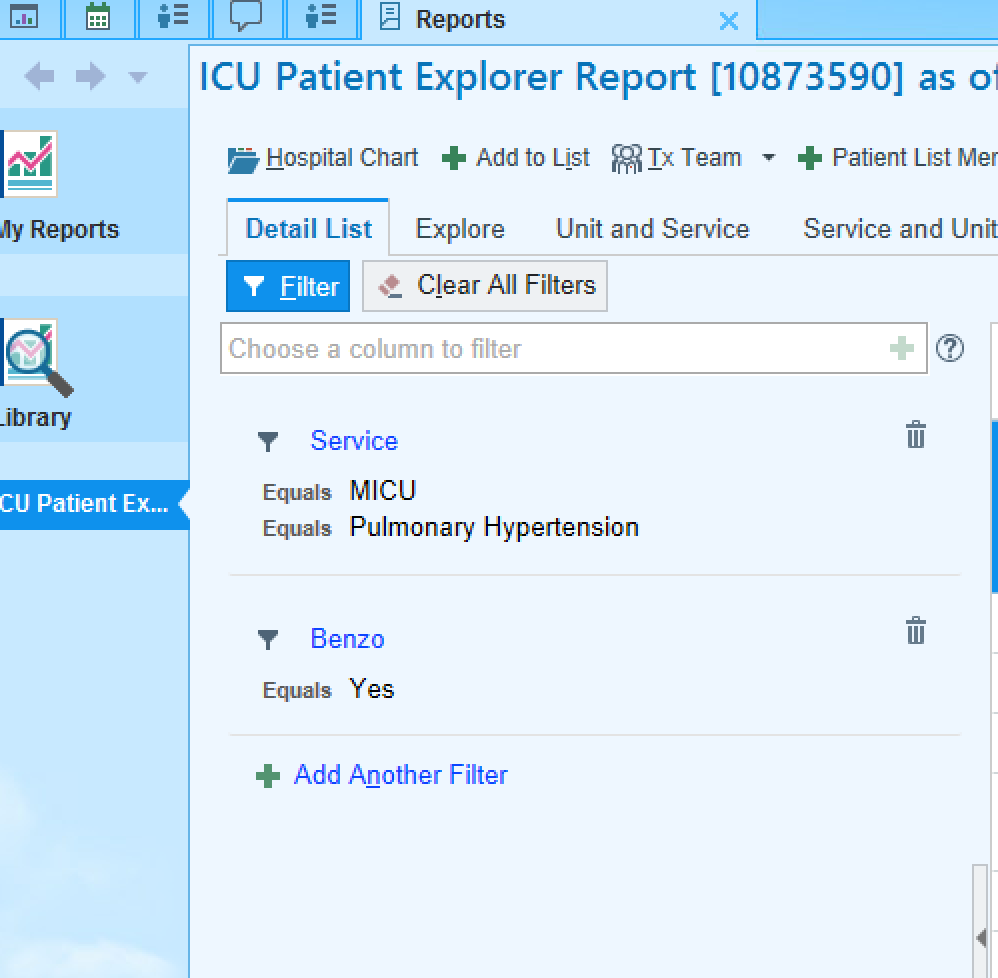
MICU C Coordination (APP team)
- Residents will work alongside the MICU C team to distribute admissions fairly by acuity and number. The MICU C team has a soft cap of ~12-14, depending on acuity. They strive to keep as close as possible to that number as possible.
- MICU C is the first call for admissions between 7am and 3pm. If MICU C is at or over their cap, if they have a high number if high-acuity patients, or if the team gets multiple admissions at once, they will give an admission to the on-call MICU A/B resident. If between 3pm and 5pm, they still have space and could finish an admission before needing to leave at 6pm, this can be discussed with them and between attendings for if they can admit a later patient.
- From 7pm to 5am, admissions will go to to the on-call MICU A/B resident. However, if the on-call resident is getting a lot of admissions at once and the MICU C team isn't at their cap, the night attending may choose to distribute an admission to the MICU C night APP. Any disputes, day or night, will be handled by faculty only.
- Please note that any cystic fibrosis or pulmonary hypertension patient should always go to the MICU A/B resident regardless of time of day; never MICU C.
- The MICU C APPs are also available to help with procedures, putting in orders, going to codes, etc. 24/7.
Codes
- Codes in the orange tower are responded to by the SICU team 24/7. After the code, it's decided which ICU is appropriate for the patient.
- Nursing staff requests that the resident running the codes (in all towers) wears a red bouffant to identify themselves as the code leader.
- The code leader will write a succinct code note describing the events of the code. Additionally, if handoff occurred to a team other than the MICU (i.e. SICU) after the code, this should be documented as well.
Service Caps
At no time should a resident or intern carry more than 10 patients.
An overcapped team should be managed by:
- buddy residents being first call and writing notes on patients, if they themselves are not overcapped;
- fellows being first call and writing notes on patients;
- redistribution of patients amongst teams;
- pulling a temporary float to help relieve the services.
Nights
The night resident must touch base with the night intensivist. If you haven't heard from the night intensivist by 7 pm, page them to confirm contact information (paging system - "CUH Night ICU Attending").
Night rounds (updated 7/6/23):
- Residents and night faculty will briefly round with the bedside nurses on the most sick/active patients on the list (including any on the admitting team's side, approximately 4-6 patients). The night intern and admitting resident should also be present as able.
- Rounds will be mainly focused on developing contingency plans and strategies to avoid emergencies overnight.
- Goals of night walk-rounds are increased support for residents/staff and more educational opportunities at night. This is not meant to be an arduous process that takes away from other patient care responsibilities.
- Rounds will occur after hand-off. This is flexible, and should occur sometime between 8-9pm depending on flow of admissions and patient care
- This will be discovery rounds style. No need to "pre-round"
Supervision
Your evaluations will be completed by the attending at the completion of the rotation. You are encouraged to solicit verbal feedback throughout the rotation as well.